Hernia-Related Heartburn: Recognizing Hiatal Hernia Symptoms
|
|
Time to read 4 min
|
|
Time to read 4 min
If you frequently experience heartburn or acid reflux that doesn’t improve with dietary changes alone, a hiatal hernia could be contributing. This article explains how hiatal hernias affect digestion, what symptoms to watch for, and how to manage them effectively.
Disclaimer: The information provided in this blog post is for general knowledge and informational purposes only, and does not constitute medical advice. Always consult with a qualified healthcare professional before making any decisions about your health or treatment. If you experience persistent or severe acid reflux, seek medical attention immediately.
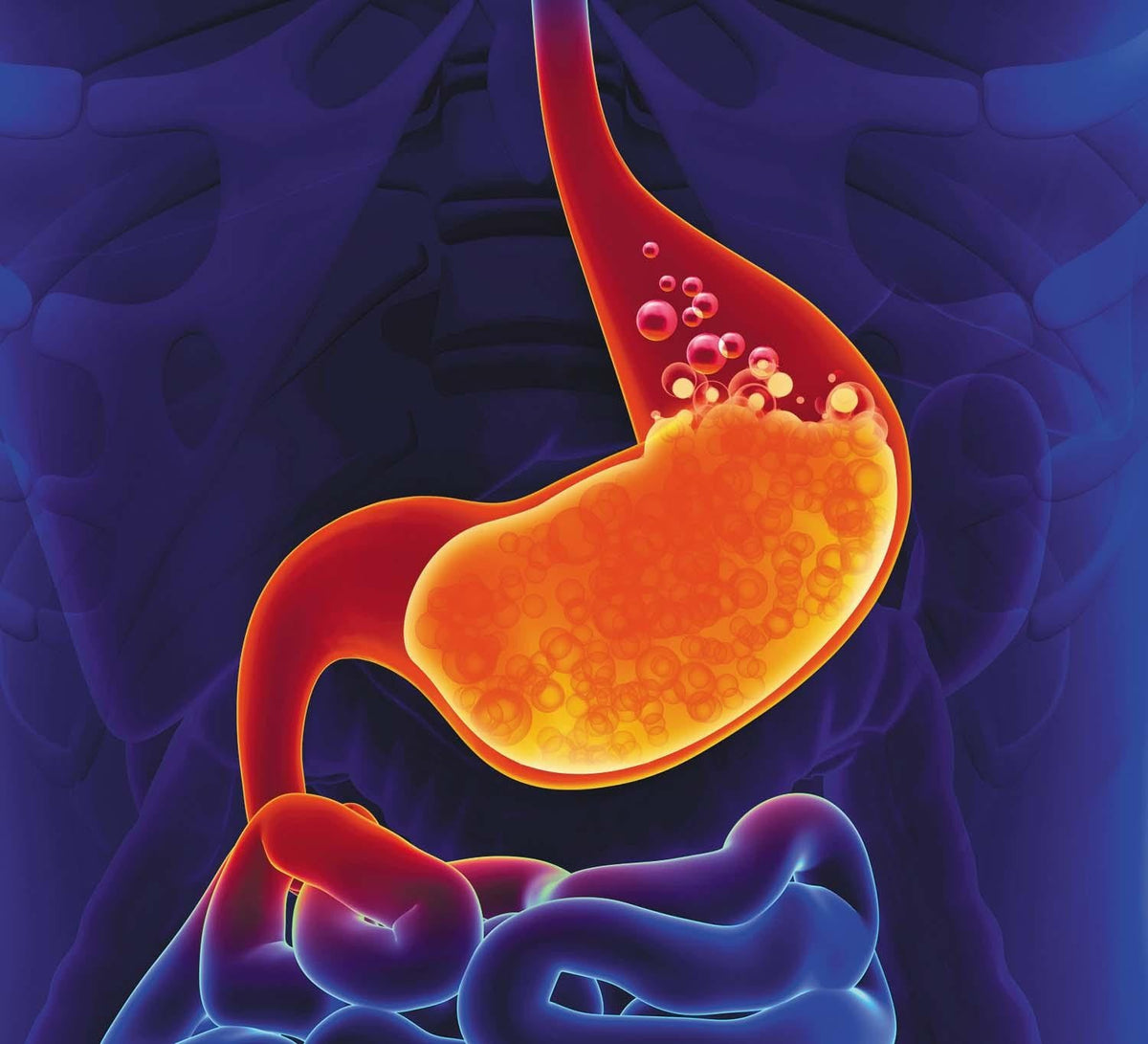
A hiatal hernia occurs when part of the stomach pushes up through the diaphragm and into the chest cavity. The diaphragm normally helps support the lower esophageal sphincter (LES), a critical barrier that prevents stomach acid from entering the esophagus.
When a portion of the stomach protrudes above the diaphragm, this support weakens. This may result in an increased likelihood of acid reflux and heartburn, especially after meals or when lying down.
Hiatal hernias can range from small and asymptomatic to large and disruptive. When symptoms do occur, they often overlap with gastroesophageal reflux disease (GERD), which can make diagnosis more complex.
Key symptoms include:
Frequent heartburn, especially after eating
Regurgitation of food or sour liquid
Feeling of fullness or pressure behind the breastbone
Difficulty swallowing (especially with larger hernias)
Occasional chest pain unrelated to the heart
Symptoms that worsen when lying down or bending over
Some individuals also experience chronic cough, hoarseness, or a sensation of a lump in the throat, particularly when acid reflux is persistent.
While occasional reflux is common, persistent or unexplained symptoms, especially if unresponsive to diet and medication, may warrant further evaluation for a hiatal hernia.
You may want to speak to your provider if:
Heartburn occurs more than twice weekly
Symptoms persist despite lifestyle changes and antacids
You experience difficulty swallowing or frequent regurgitation
Reflux is worse at night or disrupts sleep
You feel persistent upper abdominal pressure or fullness after meals
Treatment often depends on the severity of the hernia and the frequency of reflux symptoms. Many people can manage mild to moderate symptoms with non-surgical approaches.
Eat smaller, slower meals, ideally spread throughout the day.
Avoid eating within 2-3 hours of lying down.
Refrain from drinking large amounts of fluid during meals.
This approach reduces pressure on the stomach and minimizes acid reflux episodes.
Certain foods are more likely to worsen acid reflux during treatment. These may include:
Citrus fruits and juices
Tomato-based sauces
Chocolate
Fried or fatty foods
Carbonated beverages
Caffeinated drinks
Peppermint
Instead, focus on:
Lean proteins (chicken, fish, tofu)
Non-citrus fruits (bananas, melons)
Cooked vegetables
Oatmeal or whole grains
If you're unsure what your triggers are, consider keeping a food and symptom diary to track your reactions over time. You can also take Claisen’s free quiz for personalized insights into your gut health.
Avoid reclining or lying down for at least 2-3 hours after eating, as this gives gravity time to assist digestion and prevents acid from moving upward into the esophagus.
If you experience nocturnal reflux, try elevating the head of your bed by 6-8 inches or using a wedge pillow. This positioning can significantly reduce acid backflow during sleep.
Over-the-counter (OTC) and prescription drugs are available to treat acid reflux that work either by suppressing the production of stomach acid or neutralizing stomach acids. Common options include:
Calcium carbonate (e.g., Tums)
Alginate-based agents (e.g., Gaviscon)
H2 blockers (e.g., famotidine)
Proton pump inhibitors (PPIs) (e.g., omeprazole)
These reduce acid production and help manage esophageal irritation. However, they don’t correct the structural issue behind a hernia.
If symptoms persist despite medical treatment, or if complications like esophagitis or esophageal narrowing occur, surgical repair may be considered. The most common procedure is laparoscopic Nissen fundoplication, which restores LES function and repositions the stomach.
A hiatal hernia is a structural condition that increases the likelihood of acid reflux by weakening LES support.
Symptoms often overlap with GERD but may include additional signs like pressure in the chest, regurgitation, or swallowing difficulty.
Lifestyle modifications and acid suppression therapy are first-line treatments.
Surgery is reserved for severe or unresponsive cases.
Ready for personalized relief for acid reflux? Complete Claisen's gut health quiz to identify your unique reflux triggers and receive evidence-based recommendations tailored to your digestive profile.
This article and its contents have been medically reviewed by Aditya Jain (MD at Harvard Medical School and Op-Ed Fellow at Doximity).
Yes. Small hiatal hernias are often asymptomatic and may be discovered incidentally. Symptoms usually occur when acid reflux is present.
No. Most cases are managed conservatively with diet, lifestyle, and medication. Surgery is only recommended when symptoms are severe or complications arise.
Hiatal hernias do not typically resolve spontaneously. However, symptoms can often be controlled with the right management approach.


